SBC Begins Testing Donations for Rare Blood Groups
By Dr. Tho Pham, Chief Medical Officer
Did you know that many blood group systems exist beyond ABO (A, B, O and AB) and Rh (+ and -)? And that many donors have rare combinations of certain clinically relevant blood groups?
While this may come as a surprise, it may make more sense when you understand what it means to have specific blood group profiles. To provide context, a red blood cell’s surface has many carbohydrate and protein molecules on it, some of which are considered red cell antigens and are part of blood group systems. The most common antigens we hear about are the O, B, A and AB antigens which make up your ABO blood group system. The Rh factor is another important blood group system and is indicated by either (+) or (-). But many other blood group antigens exist on the red blood cell surface.
For example, the Kidd blood group system has two types: Jka and Jkb, meaning each person can be positive for both, either or neither Jka and Jkb, which occurs in varying degrees within the population. Therefore, if an O+ donor gets typed for the Kidd blood group system, writing out the donor’s extended type would like would look like: O+, Jka-, Jkb+. There are other potentially clinically relevant blood group system in addition to Kidd, such as Duffy (Fya, Fyb), Kell (K, k), and MNS (M, N, S, s).
While most patients only need blood that matches their main blood group and Rh factor (e.g., A-, AB+, O+), some patients need a much deeper level of matching — and it may not be for the reason you’d expect! For those patients who just receive one or a few transfusions, they only typically need to have their blood type matched for their main blood group because, even though they may not be a perfect match for all of the molecules on their red blood cells, it is unlikely that they will develop antibodies to all of these additional blood group antigens.
Though most patients receiving a transfusion will only need a transfusion one or a few times in their life, some patients with long-term illnesses and health conditions may require frequent transfusions for years or even a lifetime, such as individuals with sickle cell anemia, a condition in which the body produces abnormally shaped red cells that cannot transport oxygen effectively. For these chronically transfused patients, over time and with increased exposure to red blood cell antigens in the donated blood that do not match their own blood cells, their bodies start to recognize these unmatched antigens as foreign substances and can form antibodies, which ultimately leads the immune system to attack the donated red cells once they are transfused. This is dangerous for the patients since it renders the transfusion inadequate and makes the immune system attack the patient’s bloodstream.
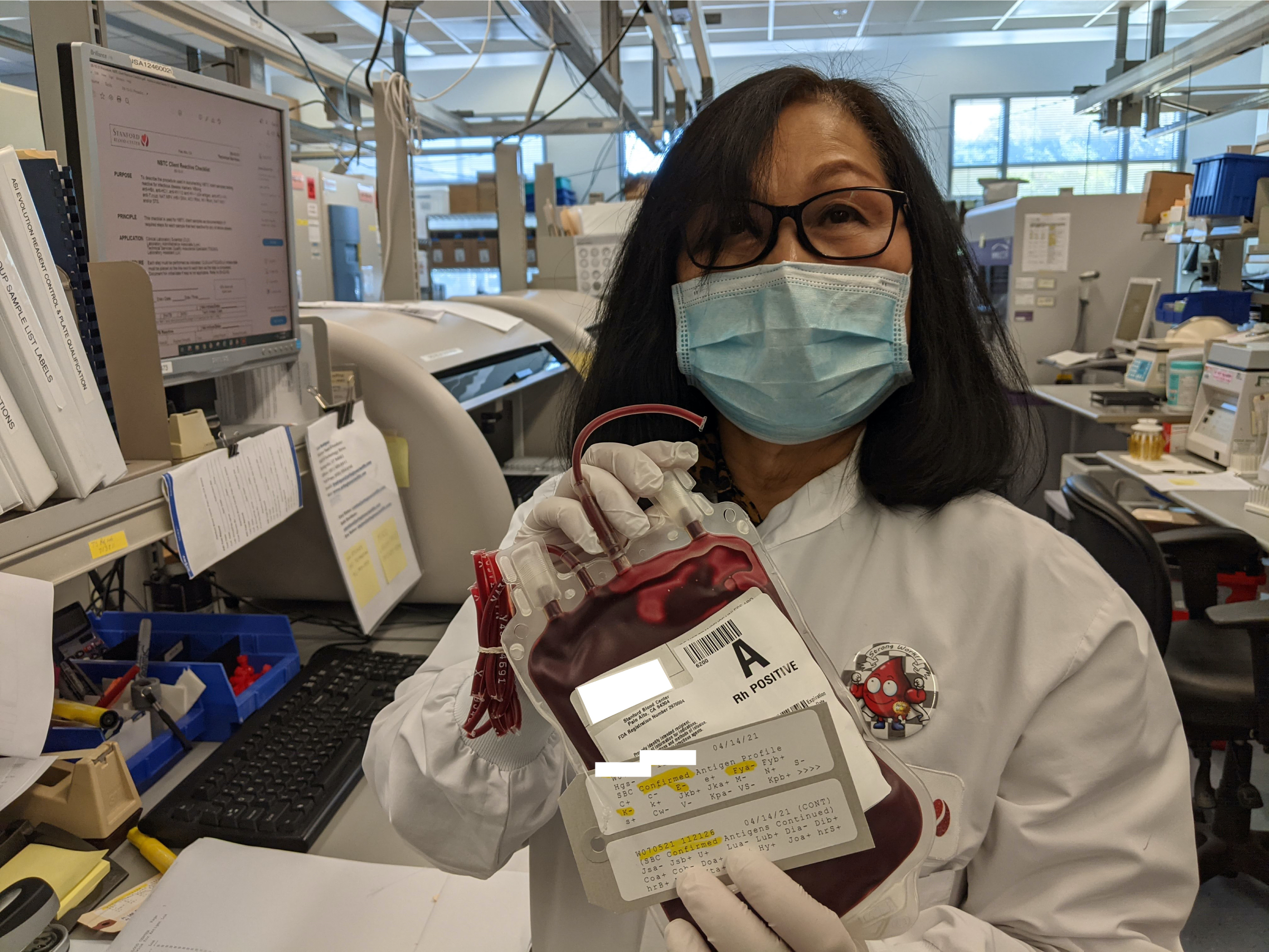
To avoid this problem, when a patient is expected to need ongoing transfusions, or when a patient has already formed antibodies against an additional red cell antigen, hospitals will do in-depth testing for these additional blood groups on the patient to determine which blood groups are present and absent. Once that profile is created, a request for a more closely matched blood donation is sent to SBC, and our Special Donations team and testing laboratory work to find a donor who may be a good match, either within SBC’s donor base or beyond, if necessary.
As you can imagine, trying to determine who would be a good match over so many blood groups can be difficult. While it may be fairly easy to find a donor who is, say, O+, or a donor who is Jka-, or a donor who is Fyb-, when you start combining all of these requirements, finding a donor who checks all the boxes in the perfect combination (O+ and Jka– and Fyb-, in this example) is often very difficult to do.
To help make this process go smoother so that we can identify matched units for these special patients quicker, earlier this year, SBC began performing more in-depth molecular type testing on blood products with red cell antigen profiles that are likely to be clinically relevant. This enables us to have information on all of these rare types ready for when a patient needs them. Currently, we run about 50 units per week through a first round of molecular testing. If the results come back clinically favorable on this first test, we will need to perform a follow-up test that allows us to confirm our results. Therefore, we will be reaching out to donors with clinical favorable and rare profiles after the first test and asking them to come back for a second donation for us to confirm the results.
While we are still in the early stages of this testing, we plan to slowly increase the number of donations that go through this screening moving forward so that we can more quickly respond to patients in need of units with rare combinations of blood groups. So, though you may not be contacted just yet, don’t be surprised if you receive a message from us saying you may have a clinically favorable and rare red cell antigen profile! If you do receive this message, we hope you will strongly consider donating again (and frequently) so that we have units available when a patient with a red cell makeup just like yours is in need of help that only someone just like you can provide!
