Blood Bag: The Unexpected Journey
Written by: Dianne Geary, technical hospital relations manager
For those of you that have donated blood before, you are familiar with the routine; the whole blood donor is asked a bunch of questions, has a mini physical and passes the test. Now he or she is led to the donor bed and lies down on the bed and tries to get comfortable. One of Stanford Blood Center’s wonderful nursing staff prepares the arm by cleaning the arm area, then unsheathes the needle and begins the phlebotomy (or pokes the person’s arm).
The donor staff fiddles with the blood bag and fills five tubes of blood and sets them with the blood bag that gently rocks on the donor scale. The donor scale stops the blood donation when the blood bag is filled. The needle is removed from the donor and the donation is sent to the segment area. The donor goes to the recovery area and has POG and cookies.
But what happens to the donation after it leaves the donor area? The mobile driver or the donor staff seals off the excess tubing from the donation bag and discards it. The blood bag and associated attached bags are wrapped up with an elastic band and placed in a cooler. The associated sample tubes are placed in the sample tube rack in Donor Information Number (DIN) numerical order. The form where all of the questions were answered by each donor is placed in a separate bag and it is locked.
The cooler of whole blood, sample tubes and questionnaires is packed up and transported to the main building of the blood center in Hillview. The tube rack is sent to the testing lab, the questionnaires are sent to Medical Records, and the whole blood donations are waiting to be manufactured in the Components lab.
Medical Records:
All of the questions that the donor answers are transferred electronically into the blood center computer system. The donor’s medical history is very private and very few people can access that information.
Testing lab:
The test tubes are spun in smaller centrifuges and each tube is sent to a different testing machine so that the testing staff only has to deal with one donor tube and not have to share donor tubes.
- One tube goes to the Nucleic Acid Testing (NAT) area where the sample tube will pipetted into small vials and put onto testing instruments that test for the smallest piece of virus present of HIV, Hepatitis B, Hepatitis C and West Nile Virus (WNV). If no virus is present, then the donor tests negative for that test.
- A separate tube goes to the testing instrument that tests for ABO, Rh and Syphilis antibodies. The blood type is electronically sent from the testing instrument to the computer system. If no antibodies to syphilis are present, then the donor tests negative for that test.
- A third tube goes to the testing instrument to see if the donor had ever been exposed to certain viral marker tests, and will check for the presence of antibodies. This instrument tests for two different strains of HIV, Hepatitis B and Hepatitis C, as well as HTLV virus. If no antibodies are present, then the donor tests negative for that test.
- A fourth tube is sent out to another testing lab that tests the donor for antibodies to T. Cruzi or Chagas’s Disease.
- The final tube is kept for a week as a retention tube-in case the tests have to be redone or if the sample tube has to be sent out for testing confirmation. Any positive viral marker test has to be sent to an alternative testing site to confirm that the donor tested positive for that test.
- All test results are entered in the donor’s record and on the donation record. Donations that test negative are ok to be released to a patient that needs it. Donations that have a positive test are retested both at SBC and at an alternate site if needed.
Components lab:
The whole blood collection set has blood in the main donor bag, and it has smaller plastic bags attached to it-either empty bags or a bag full of clear nutrient fluid. The Components tech checks the blood bag to verify that it came intact. The tech places product code labels on the blood bag to indicate what the plasma product should be made into, based on patient need.
The whole blood is placed in a centrifuge cup and then placed in a floor model centrifuge the size of a large washing machine. The blood spins and separates. The RBCs, because they are heaviest, pack to the bottom of the donation bag. The plasma, because there are no cells in it, floats on top of the RBC.
Once the centrifuge is done spinning, the whole blood is removed from the centrifuge and placed in a machine that presses on the blood bag so that the plasma will push out into one of the attached bags.
- If the blood was collected in one type of bag, all of the plasma is pushed out and a nutrient fluid stored in one of the attached bags is poured back onto the RBC so that the RBCs will last longer in the refrigerator.
- If the blood was collected in the type of bag specifically for transfusion to babies, no nutrient fluid is put back on the RBC. In these blood bags, not all of the plasma is pressed off of the RBC so the RBC can still float in donor plasma.
All extra bags are separated off from the donation bag (now the RBC bag). If the blood was collected for transfusion to babies, the RBC is placed in a refrigerator and it waits for all of the viral marker test results to be entered in the computer. If the RBCs are floating in nutrient rich fluid, then the RBC has to have the donor’s WBC filtered out of it with the attached filter. (Blood for transfusion to babies is also filtered, but it is done prior to centrifugation. It’s just how we process this type of blood bag.)
The RBC are mixed and then hung on a pole that looks like a small post or curtain hook. The tubing is opened and the blood drains to a white blood cell filter that looks like a powder puff in a compact case. The white cells stay behind in the powder puff and only the RBC drain to the final bag. The Components tech seals the tubing and leaves the tubing on the filtered RBC so the hospital can use the tubing to test if the donor’s RBC will be compatible for a future patient transfusion. Then the RBC is placed in a refrigerator that keeps the RBC at 4C/ 39F where it waits for test results as well.
The plasma product is frozen and placed in a big freezer that is -20C/ -4F or colder, then it waits until the viral marker test results are entered in the blood bank computer.
Once the testing is completed, then the RBC can be labeled and the plasma can be labeled. The Components tech scans the DIN and the product code on the RBC or plasma in the computer system.
- The computer will verify that all of the test results are in, the questionnaire is complete and that the product exists in the computer system.
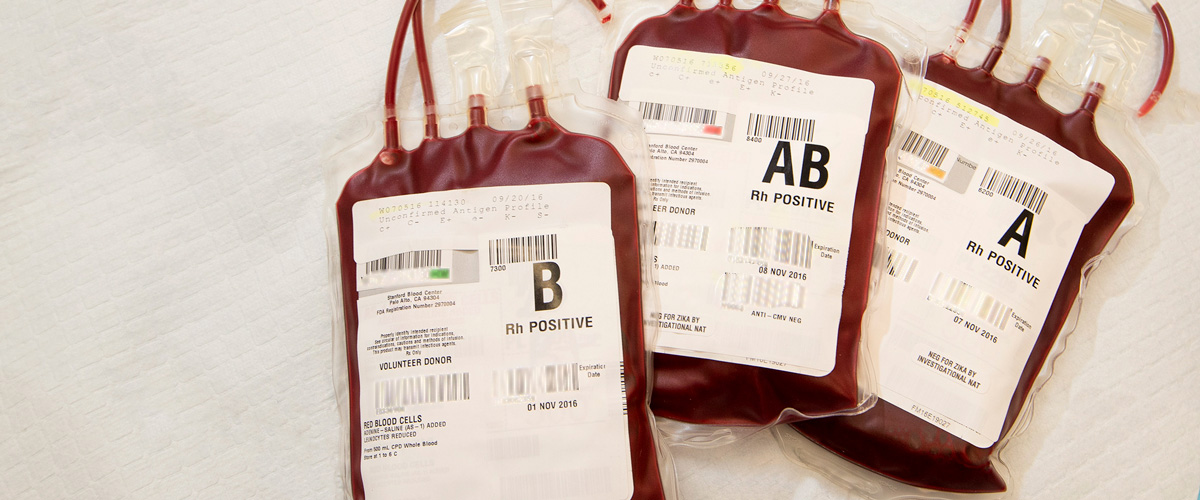
- If everything is correct, then a label is printed that covers the front of the RBC bag (or plasma bag). The label has the donor ABO/ Rh, the component product code, where the donation was manufactured, and that the donation was drawn from a volunteer donor.
- The labeled RBC is placed in a refrigerator and the plasma in a freezer. Products wait until the hospital notifies the blood center that they need to have a particular blood product and blood type available.
The hospital either calls, faxes or sends an electronic order for blood products. The Distribution Tech gets the call, fax or email and packages the blood in a cooler. The plasma products are packed on dry ice, and the RBCs are packed in a cooler with cubed ice on top. This is so the blood product maintains the RBC or plasma as close as possible to storage temperature.
The DIN, the component code, the ABO/Rh and expiration of the blood product is scanned in the computer system and it is listed as a line item on a packing list. The packing list is sent to the hospital with the blood product ordered so that they can confirm that they received it. Then the products can be used to help patients who need them! Quite the journey, indeed.
